Gastro-oesophageal reflux
What is it?
 Gastro-oesophageal reflux describes the exposure of the oesophagus to acidic secretions produced by the stomach. It is common with approximately 10% of the population experiencing weekly symptoms of heartburn or regurgitation. Almost half the population will suffer from reflux during their lifetime.
Gastro-oesophageal reflux describes the exposure of the oesophagus to acidic secretions produced by the stomach. It is common with approximately 10% of the population experiencing weekly symptoms of heartburn or regurgitation. Almost half the population will suffer from reflux during their lifetime.
Common Symptoms
- Heartburn
- Regurgitation
- Acid Brash
- Chest pain
- Cough
- Hoarseness of voice
Why does it happen?
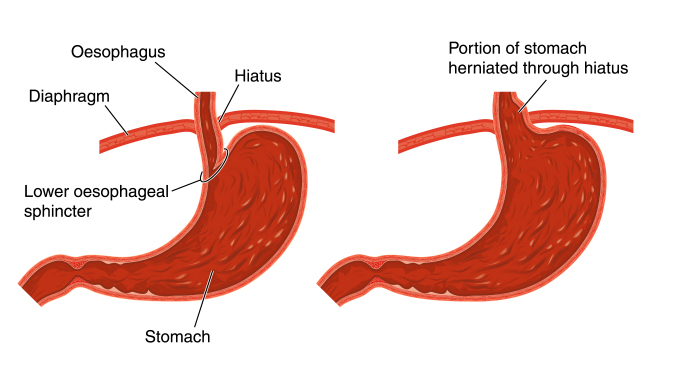
It is the result of a failure to maintain a protective reflux barrier between the oesophagus and stomach. The barrier is usually comprised of the lower oesophageal sphincter and the diaphragm muscles that surround the oesophagus. Depending on an individual’s anatomy the sphincter may not function normally or may become lax with time. This allows the passage of stomach contents into the oesophagus.
When should I seek help?
Gastro-oesophageal reflux is a common and benign condition. However, it can mask more serious underlying conditions if not investigated appropriately. Any patient with new symptoms should be reviewed, especially if associated with any difficulty in swallowing.
How is it diagnosed?
 – Gastroscopy
– Gastroscopy
Gastroscopy involves the passage of a telescope through the mouth and into the gullet. It is performed with local anaesthetic spray, with the addition of a sedative if required. The procedure assesses the lining of the oesophagus for evidence of acid injury. There maybe inflammation in the stomach and biopsies can be taken to check for conditions such as H.Pylori infection. The oesophageal lining is also checked for changes, which can progress to cancer (Barrett’s Oesophagus). This is detected by biopsies taken at the time of the procedure. It is not painful to have biopsies taken.
– Ambulatory pH Testing
Gastrooesophageal reflux is confirmed by measuring the amount of acid present in the oesophagus over a 24-48 hour period. A small capsule is placed at the bottom of the oesophagus, which then detaches and is passed spontaneously. During this time the patient carries on performing normal activities and acidic exposure is recorded. Patients also record symptoms to enable us to understand the relationship between the acid exposure and their symptoms.
– Oesophageal Manometry
Oesophageal manometry is a diagnostic test that uses tiny transducers or receivers that are integrated into a thin catheter or tube that is inserted into the oesophagus to measure pressure. This device is used to measure ability of the oesophageal sphincter to relax and to assess the motility of the oesophagus. This is a short procedure, which can be done during a visit for the pH study or as an independent investigation.
How should it be managed?
Lifestyle changes are usually the first step of management. Pregnancy, obesity, smoking and dietary factors can make symptoms worse. Patients often then find acid suppression medication helps. If prolonged medication is not suitable or fails to control the symptoms, then surgery should be considered. Prolonged symptoms, as a minimum should be investigated to exclude a more serious underlying cause. Surgery is particularly useful for patients with regurgitation.
How effective is surgery?
The LSG specializes in Anti reflux surgery in London. Surgery should be very successful provided it is performed for the correct indications. Patients should not require any more acid suppression medications and can expect immediate resolution of their symptoms. The long-term results (10 years +) are variable and some patients will restart medication again.
Are there any risks?
Patients can suffer from stomach bloating or increased flatulence (passing wind). This is due to the inability of air to escape past the new sphincter created to prevent reflux. Avoidance of fizzy drinks and certain foods may improve these symptoms. Patients are also unable to vomit, but this is not dangerous and complications from this are extremely rare. Temporary difficulty swallowing solid food can occur following anti-reflux surgery due to swelling around the oesophagus and stomach resulting from the operation. This resolves over a short period of time and it is rarely an issue long term.
How is the surgery performed?
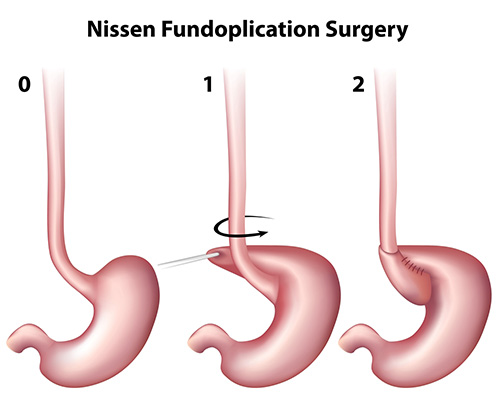 Small cuts are made in the abdominal wall to allow passage of keyhole instruments. The barrier between the oesophagus and stomach is then recreated using the ‘fundus’ of the stomach. This operation is known as a ‘fundoplication’. Fundoplication can be in a complete or partial form depending on surgical preference for each individual patient.
Small cuts are made in the abdominal wall to allow passage of keyhole instruments. The barrier between the oesophagus and stomach is then recreated using the ‘fundus’ of the stomach. This operation is known as a ‘fundoplication’. Fundoplication can be in a complete or partial form depending on surgical preference for each individual patient.
More information on Laparoscopic Surgery
How long will it take to recover from the surgery?
Patients are fully mobile after surgery and should commence fluids immediately after surgery. Often, a check contrast study is performed after the procedure before patients start a soft diet. Patients remain on a soft diet for 4 weeks to allow the postoperative swelling to settle.
Patients will often require one or two nights in hospital. This is mainly to build confidence eating and drinking after the surgery. The wound sites will have local anaesthetic injected into them at the time of surgery. This will wear off about 6 hours after the procedure. To stop the sites becoming sore you should take the regular painkillers as instructed. Shoulder tip pain is not uncommon and is due to gas underneath the diaphragm. This should not last longer than 24 hours. You will not be discharged until you are comfortable and eating and drinking. On discharge you should be independent and able to climb a flight of stairs.
Where is anti-reflux surgery performed
The LSG performs anti-reflux surgery in London (London Bridge), Surrey and Hampshire (Clare Park hospital). Please contact the practice secretary for details.
Which medications will I require after surgery?
You will be discharged from hospital with a supply of simple painkillers with instructions on how to use them. Regular paracetamol is particularly effective and can be combined with an anti-inflammatory drug (ibuprofen) or a codeine based drug (dihydrocodeine). Anti-inflammatories are not suitable for all patients and should be taken with food. The codeine-based drugs can cause constipation and should be taken with plenty of fluids. Most patients do not require painkillers after 5 days.
When can I return to work?
Generally it is recommended to take two weeks off after surgery. Your ability to return to work will depend on your job and varies between individuals. Patients can often return to work a week after surgery if required. We would not recommend flying immediately after surgery. This should be discussed on a case-by-case basis with the consultant.
When can I drive?
Driving should be avoided in the first week after surgery. Once you can perform an emergency stop in a stationary vehicle and turn to view your blind spot then driving should be safe. It is preferable to contact your insurance company to check for any specific instructions they may have.
Who do I contact if there are concerns?
The group practice telephone is answered in working hours and messages can be left out of hours. Any concerns will be relayed directly to one of the consultant surgeons on receipt. The hospital ward also provides a 24/7 means of contact. They will contact the consultant about any concerns and are able to give advice if required.
For more information on anti reflux surgery in London or anti reflux surgery in Surrey please contact us on info@londonsurgicalgroup.




